Three years after patients were given
Nobel Direct dental implants, the risk of the implant loosening has increased even more. A follow-up by researchers at the Sahlgrenska Academy in Sweden shows that
eight per cent of the implants are lost.
Nobel Direct was launched in 2004 by Nobel Biocare AB. The implants were considered a great innovation, as they could be screwed directly into the jawbone without having to first lift up the mucous membrane.
"We have followed up 48 patients who were among the first to get the implant. For each passing year, we have been able to see how the problems related to these implants have grown more and more," observes Pär-Olov Ostman, a dentist who presented the study at the defence of his dissertation.
After one year, about five per cent of the implants had been lost, and 20 per cent of the remaining implants showed bone loss of more than three millimetres. The new report indicates that after three years, eight per cent of the implants had been lost, and 25 per cent of the remaining implants showed bone loss of more than three millimetres.
"We believe that the problems related to Nobel Direct result both from the
design of the implant and an
uneven surface against the soft tissue in combination with the method of treatment recommended by the company," according to Professor Lars Sennerby.
For some time, Nobel Direct was marketed as an implant that was easy to use, and therefore suitable for
less experienced dentists. According to the company's marketing, the implant would also counteract marginal bone loss.
"If the implant is inserted in a more conservative manner, avoiding direct load, the results appear to be better. We believe that there are additional implants with similar design that can also cause problems if they are inserted in the same way as Nobel Direct. However, we are unable to draw any certain conclusions regarding these," says Professor Tomas Albrektsson, the head of the Department for Biomaterials Science at the Sahlgrenska Academy.
At the request of the Medical Products Agency, Nobel Biocare AB is now working to clarify certain information in the product information material. The company also markets several other titanium implants that have been scientifically proved to be very safe, including a Brånemark implant with the same patented surface as the Nobel Direct implant in dispute.
----------------------------
Article adapted by Medical News Today from original press release.
----------------------------
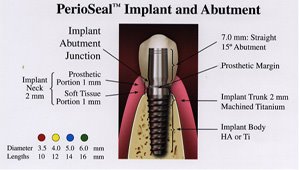
Facts about dental implants The implant is a type of artificial dental root made of titanium. The titanium screw is surgically inserted in the jawbone, and must often become well-secured there so that after several months, it can be used as a foundation for crowns, bridges and dentures. The method was invented by Professor Per-Ingvar Brånemark at the Sahlgrenska Academy in the 1960s. There are several types of titanium appliances, but all are based on titanium being a metal with the unique property of being able to be osseointegrated.
The Sahlgrenska Academy is the health science faculty of Göteborg University. Teaching and research is carried out in medicine, odontology and nursing sciences. We have about 4,000 undergraduate and 1,000 postgraduate students. Of our 1,500 employees, 850 are teachers and/or researchers.
For additional information, please contact:
Elin Lindström Claessen
Information Officer, Sahlgrenska Academy at Göteborg University
Source: Ulrika Lundin
Swedish Research Council
Main Category:
Dentistry NewsArticle Date: 02 Jan 2008 - 0:00 PST



















August 12th, 2007 at 11:51 am
When we talk about the anterior loop, we mean ‘‘an extension of the inferior alveolar nerve, anterior to the mental foramen’’. Some investigators have also referred to it as the anterior loop of the mental nerve, or described it as the mental neurovascular bundle traversing inferiorly and anteriorly to the mental foramen, which then doubles or loops back to exit the mental foramen. Detection and measurement of the anterior loop was attempted using a variety of diagnostic methods e.g. panoramic films of markers in dried skulls and cadaver mandibles, periapical films of cadaver jaws, and CT scans of patients and surgical cadaver dissections. Clinicians in doubt concerning the position of the mental foramen or who are considering placing an implant in the foraminal region at a depth where there is unease about not having a 2-mm clearance coronal to a location where an anterior loop exists should obtain a CT scan prior to implant placement to avoid injury of the inferior alveolar or mental nerve, however, the mental foramen’s location can be surgically verified. Evidence indicates that an anterior loop is present. It has been detected radiographically and by cadaver dissection; however, its size is debatable. In general, radiographic studies indicated that the anterior loop may be as long as 7.5 mm. Those who are still unwilling to accept the scientific facts can be referred to the following literature:
1) Solar P et al. A classification of the intraosseous paths of the mental nerve. Int J
Oral Maxillofac. Implants 1994; 9:339-344
2) Mardinger O. et al. Anterior loop of the mental canal: An anatomical-radiologic study. Implant Dent 2000; 9:120-125.
3) Jacobs R et al. Appearance, location, course, and morphology of the mandibular incisive canal: An assessment on spiral CT scan. Dentomaxillofac. Radiol. 2002; 31:322-327.
4) Kieser J et al. Patterns of emergence of the human mental nerve. Arch Oral Biol 2002; 47:743-747.
5) Kuzmanovic DV et al. Anterior loop of the mental nerve: A morphological and radiographic study. Clin Oral Implants Res 2003; 14:464-471
6) Jacobs R, et al. Appearance of the mandibular incisive canal on panoramic radiographs. Surg Radiol. Anat. 2004; 26:329-333.